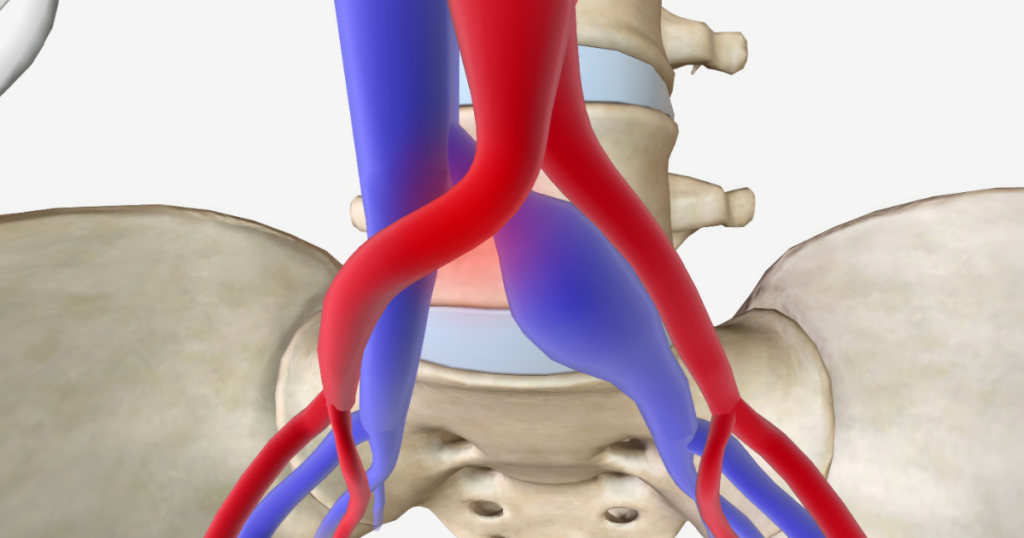
May-Thurner Syndrome (MTS) is a condition that occurs when the right iliac artery compresses the left iliac vein in the pelvic region. This compression can obstruct the flow of blood, leading to various symptoms, and may even cause more severe complications if left untreated.
The condition is named after Dr. May and Dr. Thurner, who first identified the association between the iliac artery and vein in the 1950s. MTS can lead to venous problems, including chronic pain, swelling, and in some cases, the development of blood clots, especially in the left leg. While MTS is rare, understanding the condition is crucial for effective diagnosis and management.
What Causes May-Thurner Syndrome?
May-Thurner Syndrome is primarily caused by the compression of the left iliac vein by the right iliac artery. The iliac veins are responsible for carrying deoxygenated blood from the legs back to the heart, while the iliac arteries carry oxygen-rich blood to the legs. In MTS, the right iliac artery crosses over and compresses the left iliac vein, which impairs blood flow, causing the blood to pool in the veins of the lower extremities.
Several factors contribute to the development of MTS, including:
- Anatomical abnormalities: Some individuals may be born with an inherent anatomical predisposition where the right iliac artery is positioned unusually high, causing increased pressure on the left iliac vein.
- Trauma or injury: Any injury or trauma to the pelvic area may lead to scarring or changes in vascular structures that cause compression.
- Age: As people age, vascular structures may undergo changes that increase the risk of vein compression.
- Other health conditions: Obesity, pregnancy, or deep vein thrombosis (DVT) can increase the likelihood of developing MTS, as they may exacerbate venous insufficiency and pressure on the veins.
The condition is more common in women, especially those of reproductive age, due to hormonal changes and anatomical differences in the pelvic area. However, it can affect both men and women across all age groups.
Symptoms of May-Thurner Syndrome
The symptoms of May-Thurner Syndrome vary from person to person. In some individuals, there may be no noticeable symptoms, while others may experience moderate to severe manifestations. Symptoms commonly associated with MTS include:
- Leg swelling: Swelling, especially in the left leg, is the most common symptom. The swelling occurs due to poor blood flow and the accumulation of fluid in the lower extremities.
- Pain and discomfort: Individuals with MTS often report persistent pain, aching, or cramping in the affected leg, especially after standing or sitting for prolonged periods.
- Skin discoloration: The skin on the affected leg may become discolored, ranging from a reddish or purple hue to a darker shade, due to poor circulation and blood pooling.
- Heaviness or fatigue: The legs may feel unusually heavy or fatigued, making it difficult to walk or perform daily activities.
- Numbness or tingling: In some cases, individuals with MTS may experience sensations of numbness or tingling in the affected leg as a result of impaired circulation.
- Reduced mobility: The swelling and pain associated with MTS can limit mobility, making it difficult to walk or climb stairs.
In more severe cases, MTS can lead to complications such as the formation of deep vein thrombosis (DVT), which is a blood clot that can travel to the lungs and cause a pulmonary embolism. This is a medical emergency and requires immediate treatment.
Diagnosis of May-Thurner Syndrome
To diagnose May-Thurner Syndrome, a healthcare provider will typically start by reviewing the patient’s medical history and performing a physical examination. However, because MTS shares symptoms with other conditions, specialized imaging tests are necessary for a definitive diagnosis.
The following diagnostic tools are commonly used:
- Doppler ultrasound: A non-invasive test that uses sound waves to create an image of blood flow in the veins. It can detect blood clots and changes in blood flow caused by compression.
- CT or MRI venography: A more advanced imaging technique that provides detailed images of the veins and arteries in the pelvic region. This helps identify the compression of the left iliac vein.
- Angiography: In some cases, a contrast dye may be injected into the veins to provide clear imaging of blood flow and confirm the diagnosis of MTS.
In addition to these tests, the physician may order blood tests to check for any clotting abnormalities, especially if there is concern for deep vein thrombosis (DVT).
Treatment Options for May-Thurner Syndrome
Treatment for May-Thurner Syndrome depends on the severity of the condition and the symptoms experienced by the patient. A range of options is available to manage the condition and improve quality of life.
Lifestyle Modifications
For individuals with mild symptoms, lifestyle changes may help alleviate some of the discomfort. These can include:
- Leg elevation: Elevating the legs regularly can help reduce swelling and improve blood circulation.
- Compression stockings: Wearing compression stockings can help reduce swelling and improve venous circulation.
- Physical activity: Regular exercise, especially walking or swimming, can promote circulation and prevent further complications.
Medications
In some cases, medications may be prescribed to reduce inflammation, alleviate pain, or prevent blood clots. Blood thinners (anticoagulants) may be used to prevent DVT, while pain relievers may help manage discomfort.
Endovenous Treatment
For more severe cases, minimally invasive procedures may be recommended. One common treatment is endovenous stenting, where a stent is placed in the left iliac vein to keep it open and allow normal blood flow. This procedure is often performed under local anesthesia and has a high success rate in relieving symptoms and preventing recurrence.
Surgical Options
In rare cases where conservative treatments are not effective, surgical intervention may be necessary. This can involve vein bypass surgery or removing the compressed portion of the iliac vein.
Long-Term Management and Living with May-Thurner Syndrome
Living with May-Thurner Syndrome can be challenging, but with proper treatment and management, individuals can lead healthy and active lives. Key components of long-term management include:
- Regular check-ups: It is important to monitor symptoms regularly and have follow-up appointments with a vascular specialist to assess the effectiveness of treatment.
- Self-care: Maintaining a healthy weight, staying active, and avoiding prolonged periods of immobility are essential for managing MTS. In addition, wearing compression stockings as recommended and elevating the legs can help manage symptoms.
- Managing pain and swelling: Consistent use of compression garments and elevating the legs can prevent swelling from worsening. If pain becomes severe, medical intervention may be necessary.
What Is the Long-Term Outlook for People with May-Thurner Syndrome?
The long-term outlook for people with May-Thurner Syndrome is generally positive with proper treatment. Early detection and intervention are key to preventing complications like blood clots or chronic venous insufficiency. People who follow their doctor’s treatment plan, make necessary lifestyle changes, and maintain regular check-ups can manage their condition effectively.
Living with May-Thurner Syndrome
There are many resources available for individuals living with May-Thurner Syndrome. Patients can connect with support groups, both online and in-person, to share experiences and learn about effective coping strategies. Additionally, healthcare providers and vascular specialists can offer valuable information and direct patients to appropriate resources.
If you are experiencing symptoms of May-Thurner Syndrome or have been diagnosed, it’s important to speak with a healthcare provider to discuss treatment options and create a management plan tailored to your needs. Regular monitoring, early intervention, and a healthy lifestyle are crucial in managing MTS successfully.
May-Thurner Syndrome is a complex condition that can cause significant discomfort and lead to complications if left untreated. However, with early diagnosis, effective treatment, and ongoing management, individuals with MTS can live active, fulfilling lives. If you suspect you may have May-Thurner Syndrome or are experiencing symptoms, consult with a vascular specialist to explore your options for diagnosis and treatment.
Schedule Your Vein & Vascular Consultation
Take the first step toward better circulation and healthier legs. Our board-certified specialists provide minimally invasive treatments for varicose veins, poor circulation, and vascular conditions—most procedures take just 20-30 minutes.
Frequently Asked Questions
Pain from May-Thurner Syndrome typically feels like aching, heaviness, or cramping in the affected leg, often worsened by standing or sitting for long periods. Some individuals also experience swelling, fatigue, or discomfort.
May-Thurner Syndrome can be mistaken for other conditions like deep vein thrombosis (DVT), chronic venous insufficiency, or varicose veins, as they share symptoms like leg pain, swelling, and discomfort. Schedule a consultation with one of our specialists at United Vein & Vascular Centers today to get a proper diagnosis and explore your treatment options.
May-Thurner Syndrome does not have universally defined “stages,” but it can be considered in terms of severity: mild (occasional swelling and discomfort), moderate (persistent swelling and pain), and severe (chronic swelling, blood clots, or significant venous insufficiency).


