Hot To Prevent Blood Clots If You Suffer with CVI
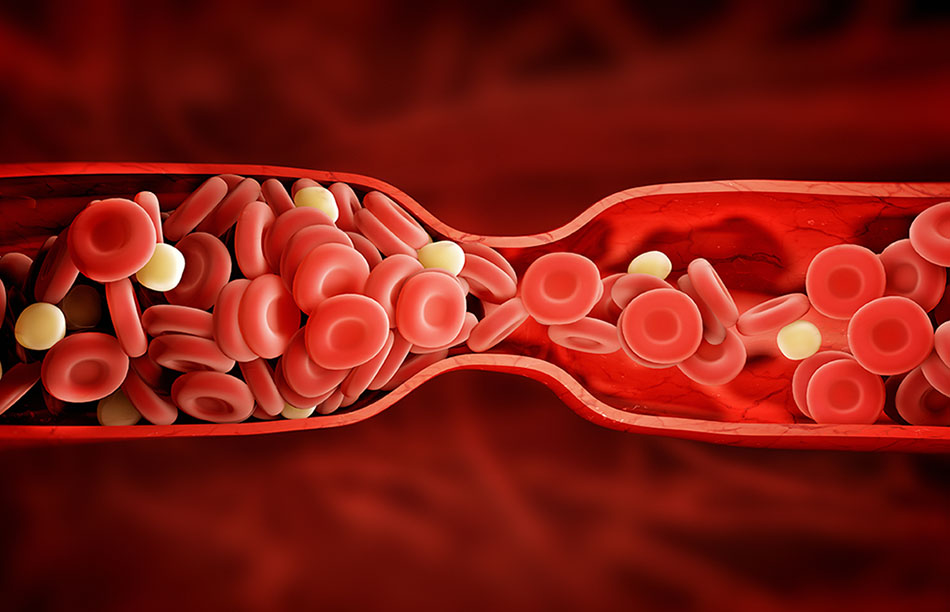
Chronic venous insufficiency (CVI) is a condition where the veins in the legs become damaged and don’t perform as well as they should. It is considered a venous disease that negatively affects blood flow and disrupts the ability of the body to circulate blood efficiently. This venous disease is most relevant for older adults, particularly those over 50. There is a connection between chronic venous insufficiency and deep vein thrombosis (DVT), which is the medical term for blood clots. Those who have CVI face a significantly higher risk of developing DVT.
To learn more about how CVI patients can prevent the development of blood clots in their legs, read the information below.
How can CVI patients prevent blood clots from developing?
- Get regular exercise — Making sure to get some body movement in every day is a good way to boost circulation and prevent the development of blood clots. However, patients who have already developed a blood clot may need to be cautious about exercising, which can cause the clot to travel to the lungs.
- Take blood-thinning medication — Blood thinners can be prescribed to patients with chronic venous insufficiency to prevent developing blood clots. They are also prescribed to break up blood clots when they have already formed.
What are some treatment options for chronic venous insufficiency?
- Endovenous laser ablation — Endovenous laser ablation is one of the methods that vascular specialists may use to close the damaged veins that result from CVI. During this minimally invasive procedure, a small laser is used on the veins to seal them and reroute blood flow to healthier veins.
- Microphlebectomy — A microphlebectomy is another minimally invasive procedure that can be used to remove damaged veins from the legs. During this procedure, a small hooklike instrument is inserted through a tiny incision and the damaged veins are pulled out.
Contact United Vein & Vascular Centers for your vein condition
You don’t have to continue worrying about symptoms of vein conditions that are making your life more difficult. Our vein specialists at United Vein & Vascular Centers are here to help you. Each of our team members understands the uncertainty and discomfort that vein problems can lead to, and that’s why they’re committed to helping you better understand your condition, your symptoms, and the options you can use to address them.
Our specialists can also help you find the most effective treatment option for your vein condition and include it in a comprehensive treatment plan that’s designed to:
- Reduce your symptoms.
- Improve your ability to walk and perform other normal daily tasks.
- Increase your overall quality of life.
Contact us today to learn more about your vein condition and the ways it can be treated or to set up an initial appointment.