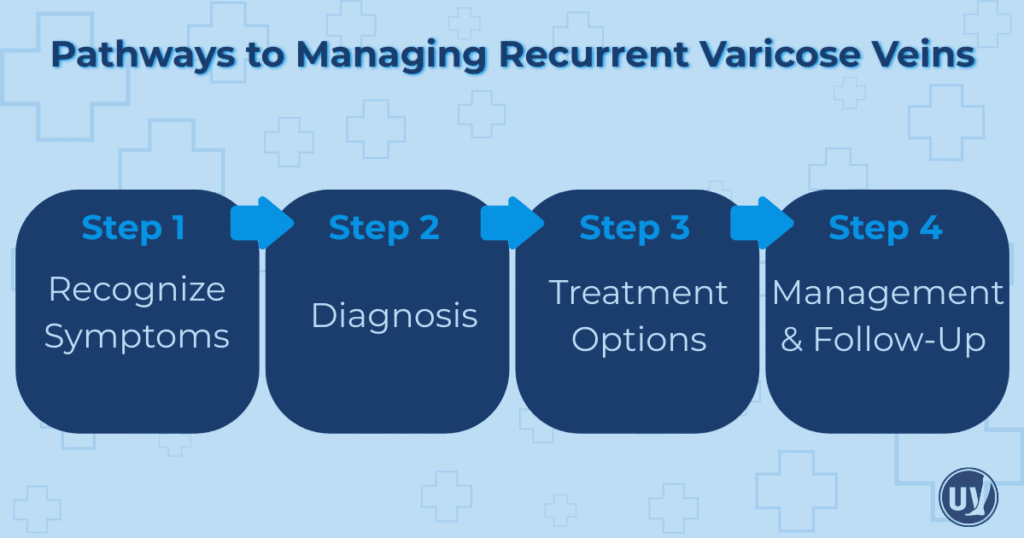
Recurrent varicose veins can be frustrating, painful, and discouraging. Many patients find that even after undergoing treatment, veins may reappear or new ones may develop. Understanding why varicose veins return is essential for managing the condition effectively and preventing further complications. Recurrence can be influenced by a variety of factors, including incomplete treatment, genetics, lifestyle habits, and underlying vein health.
While varicose veins are often viewed as a cosmetic concern, they are more than skin-deep. Symptoms such as swelling, aching, heaviness, and visible bulging veins can interfere with everyday activities, mobility, and overall quality of life. Early recognition of these symptoms and proactive management are key to improving vein health and preventing more serious complications. Fortunately, patients today have a wide range of treatment options, from lifestyle modifications to advanced minimally invasive procedures and surgical interventions.
By understanding recurrent varicose veins and exploring the most effective treatment paths, you can take control of your vein health, reduce discomfort, and enhance your overall well-being.
Understanding Recurrent Varicose Veins
Recurrent varicose veins are veins that reappear after previous treatment, either in the same location or in new areas of the leg. Recurrence can occur for several reasons, including incomplete initial treatment or the development of new veins in untreated areas. Genetic predisposition also plays a major role, as individuals with a family history of varicose veins are more likely to experience recurrence.
Lifestyle factors such as prolonged standing or sitting, obesity, pregnancy, and hormonal changes can further increase the risk of veins returning. Patients may notice the same symptoms they experienced previously: aching, swelling, heaviness, or visibly bulging veins. These symptoms can disrupt daily activities, reduce mobility, and affect overall comfort. Understanding why veins return allows patients to take proactive steps to prevent further recurrence and work with healthcare providers to develop effective treatment plans.
Causes and Risk Factors
Several factors contribute to the recurrence of varicose veins. Some, like genetics, are beyond your control, while others, such as lifestyle habits, can be managed to reduce risk. A family history of varicose veins significantly increases the likelihood of recurrence, making early intervention and proactive care especially important.
Lifestyle factors that contribute to recurrence include prolonged periods of standing or sitting, which increase pressure in the veins of the legs. Obesity and pregnancy also place extra strain on the veins, creating an environment where varicose veins are more likely to return. Hormonal fluctuations, particularly during pregnancy or menopause, can further affect vein health and circulation.
Incomplete initial treatment is another common factor. If all problematic veins are not fully addressed during the first treatment, they may become symptomatic again. Additionally, lack of regular follow-up care can allow small vein issues to progress into more noticeable or painful varicose veins. By understanding these risk factors, patients can adopt preventive strategies and work closely with their healthcare providers to monitor vein health.
Recognizing Symptoms and Seeking Help
Early recognition of recurrent varicose veins is vital to effective management. Symptoms often include aching, throbbing, heaviness, and swelling in the legs. These sensations may worsen after standing or sitting for long periods. Visibly bulging, twisted veins are another common sign. In some cases, the skin over affected veins may darken, become discolored, or show textural changes.
Seeking medical attention as soon as symptoms appear is essential. Persistent swelling, severe pain, or the formation of skin ulcers warrants prompt evaluation. Early intervention can reduce discomfort, prevent complications, and improve long-term outcomes. A vein specialist can assess the condition, recommend diagnostic tests, and guide patients toward the most appropriate treatment options.
Diagnosing Recurrent Varicose Veins
Accurate diagnosis is a crucial step in treating recurrent varicose veins. Vein specialists rely on advanced imaging techniques to evaluate blood flow, detect underlying vein dysfunction, and identify the specific veins contributing to symptoms. Duplex ultrasound is the primary diagnostic tool, providing detailed images of vein structure and blood flow patterns. This non-invasive test helps specialists determine which veins require treatment.
In some cases, additional imaging, such as MRI scans or CT venography, may be recommended to provide a more comprehensive view of the vascular system. Accurate diagnosis allows for a personalized treatment plan tailored to the patient’s specific needs, increasing the likelihood of successful outcomes and reducing the risk of future recurrence.
Initial Management Strategies
The first steps in managing recurrent varicose veins often involve lifestyle changes and non-invasive interventions. Regular physical activity, such as walking, swimming, or low-impact exercise, encourages healthy circulation in the legs. Maintaining a healthy weight reduces pressure on the veins, while elevating the legs periodically throughout the day can help alleviate swelling and discomfort.
Compression therapy is another essential component of initial management. Compression stockings apply consistent pressure to support the veins, improve blood flow, and reduce swelling. These non-invasive approaches can alleviate symptoms, prevent further vein deterioration, and set the foundation for more advanced treatments if needed.
Minimally Invasive Treatment Options
For patients whose symptoms persist despite lifestyle adjustments, minimally invasive procedures provide effective solutions with minimal downtime. Sclerotherapy involves injecting a solution directly into the vein, causing it to close and gradually fade. This treatment is especially effective for smaller varicose veins and spider veins.
Endovenous Laser Therapy (EVLT) is another option that uses laser energy to seal larger veins from within. This technique is precise, minimally invasive, and often provides rapid symptom relief. Radiofrequency Ablation (RFA) is a similar approach, utilizing heat delivered through a catheter to close problematic veins. These treatments are generally well-tolerated, allowing patients to return to normal activities quickly while achieving both functional and cosmetic improvement.
Surgical Approaches
In more severe cases, surgery may be required. Vein stripping and ligation involves removing or tying off sections of the affected veins, while ambulatory phlebectomy targets smaller surface veins through tiny skin punctures. Surgical treatments are typically performed under local anesthesia, and recovery times vary, though most patients resume normal activities within a few weeks. Consulting with a vein specialist ensures the chosen surgical approach aligns with the patient’s specific needs and overall health goals.
Long-Term Management and Lifestyle Adjustments
Sustaining vein health over the long term requires attention to lifestyle and preventive strategies. Regular exercise promotes circulation, maintaining a healthy weight reduces strain on the veins, and elevating the legs throughout the day helps reduce pressure. A balanced diet rich in fiber, fruits, and vegetables also supports overall vascular health.
Compression therapy, whether through stockings or specialized wraps, can aid blood flow and prevent swelling. Regular monitoring and follow-up with a vein specialist ensure that any new or recurring veins are addressed promptly, reducing the likelihood of complications. These combined efforts help manage symptoms, prevent recurrence, and enhance long-term comfort.
Follow-Up Care and Monitoring
Preventing further recurrence relies on consistent follow-up and monitoring. Routine visits with a healthcare provider, along with diagnostic imaging when needed, help track vein health and detect early signs of recurrence. Promptly addressing any new symptoms allows patients to maintain optimal circulation and prevent minor issues from becoming more serious. A proactive approach, guided by a qualified specialist, is the key to sustained vein health.
Empowering Your Vein Health Journey with UVVC
Living with recurrent varicose veins can feel overwhelming, but you don’t have to manage it alone. At United Vein & Vascular Centers (UVVC), our team of specialists is dedicated to helping patients find relief through personalized treatment plans. Whether you need minimally invasive procedures, surgical options, or guidance on lifestyle and long-term management, UVVC provides comprehensive care tailored to your needs.
By understanding your vein health, recognizing symptoms early, and partnering with experienced professionals, you can take control of your vascular health. Don’t wait for symptoms to worsen—schedule a consultation with UVVC today to explore treatment options and take the first step toward healthier, more comfortable legs.
Frequently Asked Questions
Varicose veins can recur due to incomplete treatment, genetic predisposition, new vein formation, or lifestyle factors like prolonged standing, obesity, and hormonal changes. Understanding the cause helps guide effective management.
Treatment options include lifestyle adjustments, compression therapy, minimally invasive procedures such as sclerotherapy, endovenous laser therapy (EVLT), and radiofrequency ablation (RFA), as well as surgical approaches like vein stripping and ambulatory phlebectomy for more severe cases.
Maintaining healthy circulation through regular exercise, managing weight, elevating legs, wearing compression stockings when recommended, and attending regular follow-ups with a vein specialist can significantly reduce the risk of varicose veins returning.


