Knee Osteoarthritis: Causes, Symptoms, Diagnosis, and Treatment
What Is Knee Osteoarthritis?
Knee osteoarthritis is a common joint condition that occurs when the protective cartilage cushioning the ends of the bones gradually wears down. As this cartilage breaks down, the bones in the knee joint can begin to rub against each other, leading to inflammation, stiffness, and pain. Over time, the joint may become less flexible and more difficult to move, making everyday activities like walking, climbing stairs, or standing for long periods increasingly uncomfortable. Knee osteoarthritis often develops slowly and may worsen with age, previous injuries, or long-term stress on the joint.

Request a Consult

Symptoms of Knee Osteoarthritis
The symptoms of knee osteoarthritis often develop gradually and may worsen over time as joint inflammation and cartilage damage progress. While the severity of symptoms varies from person to person, many patients notice increasing discomfort that begins to interfere with daily activities.
Common symptoms of knee osteoarthritis include:
- Persistent knee pain that worsens with movement or weight-bearing activities
- Stiffness in the joint, especially in the morning or after sitting for long periods
- Swelling around the knee caused by inflammation
- Tenderness when pressing on the joint
- A grinding, popping, or clicking sensation during movement
- Reduced range of motion or difficulty fully bending or straightening the knee
- Pain when walking, climbing stairs, kneeling, or standing for extended periods
As the condition progresses, pain may become more constant and mobility may decrease, making routine tasks more challenging. Some individuals also experience flare-ups where symptoms temporarily become more severe.

What Causes Knee Osteoarthritis Pain?
Knee osteoarthritis pain develops from a combination of joint damage and inflammation. As the protective cartilage in the knee wears down, the bones begin to move less smoothly against each other. This increased friction can irritate the joint, leading to swelling, stiffness, and discomfort during movement.
Inflammation plays a major role in ongoing pain. When the joint becomes inflamed, the lining of the knee produces chemicals that increase sensitivity and contribute to persistent soreness. Over time, the body may also form tiny new blood vessels in the irritated tissues surrounding the joint. These vessels can bring additional inflammatory signals to the area, which may intensify pain and make symptoms harder to manage with conservative treatments alone. In some cases, minimally invasive treatments can target this inflammation directly.
Because knee osteoarthritis pain can stem from both structural changes and chronic inflammation, symptoms may continue even after rest, medication, or basic therapies. Understanding these underlying causes helps guide treatment decisions and determine when additional options may be appropriate.

How Knee Osteoarthritis Is Diagnosed
Diagnosing knee osteoarthritis typically begins with a medical evaluation and a review of your symptoms. A healthcare provider will ask about your pain, stiffness, mobility changes, and how your knee discomfort affects daily activities. They may also examine the joint to check for swelling, tenderness, range of motion, and signs of joint instability.
Imaging tests are often used to confirm the diagnosis and assess the severity of joint damage. X-rays can show narrowing of the joint space, bone changes, and cartilage loss that are common with osteoarthritis. In some cases, an MRI may be recommended to provide a more detailed view of the soft tissues, including cartilage, ligaments, and the joint lining.
An accurate diagnosis helps determine the stage of osteoarthritis and guides decisions about the most appropriate treatment options to relieve pain and improve mobility.
Common Treatment Options for Knee Osteoarthritis
Treatment for knee osteoarthritis usually begins with conservative approaches aimed at reducing pain, improving mobility, and slowing the progression of joint damage. The right treatment plan depends on the severity of symptoms, lifestyle factors, and overall health.
Common non-surgical treatment options include:
- Physical therapy and exercise to strengthen the muscles around the knee and improve joint stability
- Weight management, which can reduce stress on the knee joint and lessen pain
- Anti-inflammatory medications to help control swelling and discomfort
- Bracing or supportive devices to improve alignment and reduce strain on the joint
- Corticosteroid or hyaluronic acid injections to provide temporary relief from inflammation and stiffness
For many people, these treatments can help manage symptoms for a period of time. However, as osteoarthritis progresses, pain may become more persistent and daily activities may become increasingly difficult despite these efforts. When conservative treatments no longer provide adequate relief, additional options may be considered.

When Conservative Treatments Are Not Enough
While many people find relief with physical therapy, medications, or injections, these approaches do not always provide long-term improvement. As knee osteoarthritis progresses, pain may become more frequent, mobility may decrease, and everyday activities like walking, standing, or climbing stairs can become increasingly difficult.
When conservative treatments no longer control symptoms, it may be time to explore additional options. Some patients consider knee replacement surgery, but others may not be ready for a major operation or may not be good candidates due to age, activity level, or other medical conditions.
In certain cases, minimally invasive Genicular Artery Embolization may be recommended to help reduce pain and inflammation within the joint. These treatments are designed to target the sources of chronic knee pain without the need for open surgery and may help patients delay or avoid joint replacement. A specialist can evaluate your condition and determine whether an advanced treatment approach may be appropriate for you.

Minimally Invasive Treatment for Knee Osteoarthritis Pain
For many people, knee osteoarthritis pain continues even after trying medications, physical therapy, braces, or joint injections. When conservative treatments no longer provide relief — but you are not ready for knee replacement surgery — a minimally invasive option may help.
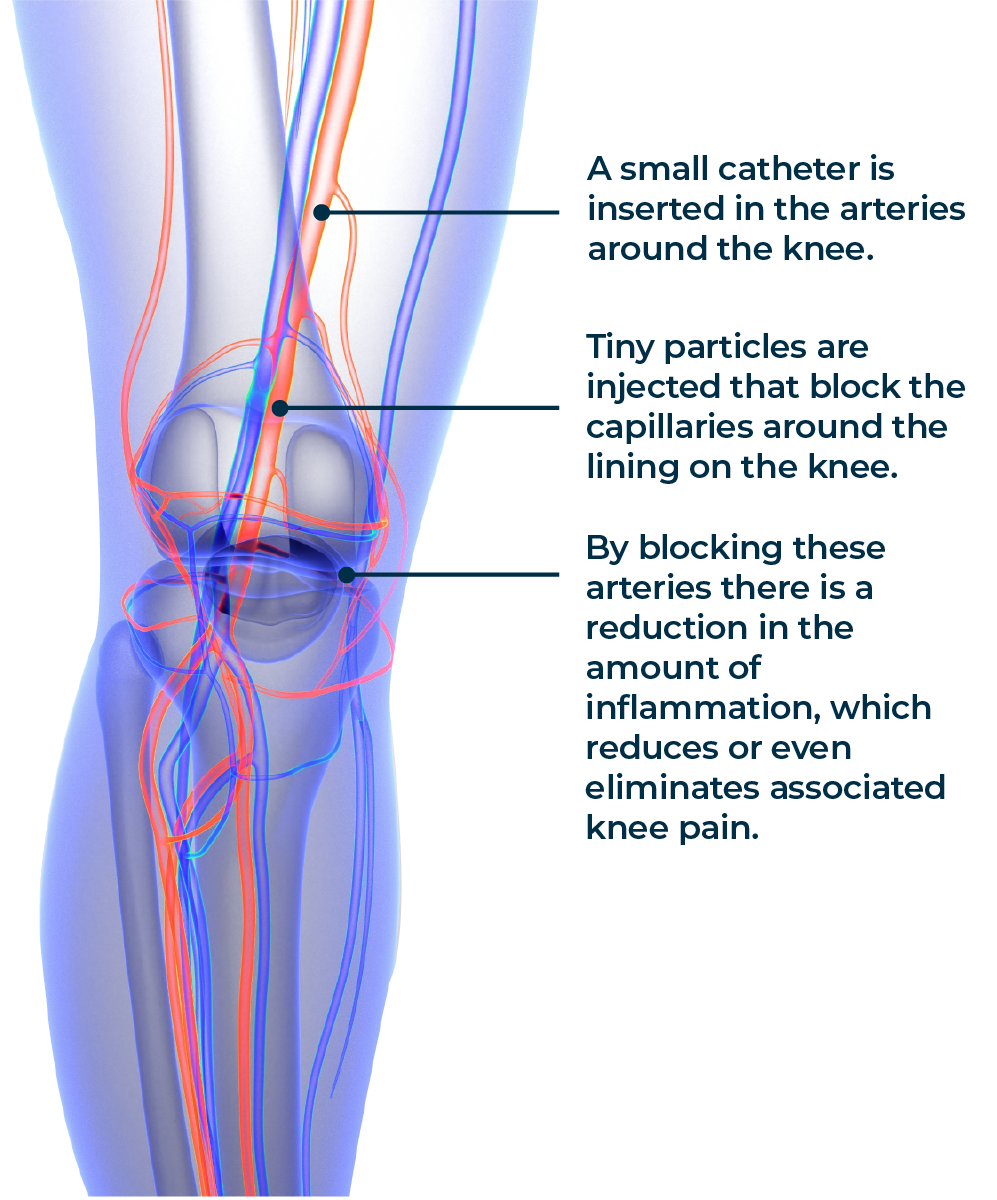
Genicular Artery Embolization (GAE) is an advanced, image-guided procedure designed to reduce inflammation inside the knee joint. In osteoarthritis, tiny abnormal blood vessels develop in the lining of the knee. These vessels contribute to ongoing inflammation and pain. GAE works by blocking these vessels, which helps calm the inflammation and significantly reduce discomfort.
Unlike knee replacement surgery, GAE:
- Does not require large incisions
- Is performed through a tiny puncture in the groin or wrist
- Allows patients to go home the same day
- Has a much shorter recovery time
Many patients experience meaningful pain relief within weeks of the procedure and improved ability to walk, exercise, and perform daily activities.
GAE can be an excellent option for people who want to stay active, delay joint replacement, or avoid major surgery altogether.
