Contents
- What Is Chronic Venous Insufficiency?
- Causes and Risk Factors of Chronic Venous Insufficiency
- Recognizing the Symptoms: Early and Advanced Stages
- Understanding the Progression of Chronic Venous Insufficiency
- Leg Swelling Causes and How They Relate to CVI
- Diagnosis: How Chronic Venous Insufficiency Is Identified
- Venous Insufficiency Treatment Options
- Preventing Progression and Complications
- When to See a Vein Specialist
- Empowering Patients: Taking Charge of Your Vein Health
- Frequently Asked Questions
Chronic venous insufficiency (CVI) affects millions of people, yet it’s often misunderstood. When the veins in your legs struggle to return blood to the heart, it can cause uncomfortable symptoms like swelling, aching, and fatigue, impacting your daily life more than you might realize.
Understanding CVI is the first step toward managing it effectively. From subtle early signs to more advanced symptoms, knowing what to look for and when to seek treatment can make all the difference.
Empower yourself with knowledge and discover how early intervention can improve your comfort and quality of life.
What Is Chronic Venous Insufficiency?
Chronic venous insufficiency (CVI) is a condition affecting the veins in your legs. These veins struggle to send blood back to your heart efficiently. This is often due to malfunctioning valves within the veins.
In healthy veins, valves open and close to help blood flow. When these valves become damaged or weakened, blood can pool in the legs. This pooling increases pressure in the veins, leading to various symptoms.
Common symptoms of CVI include:
- Leg swelling and pain
- A feeling of heaviness in the legs
- Varicose veins and skin changes
Understanding CVI’s impact on your body can help in recognizing symptoms early. Early diagnosis and treatment are crucial to prevent worsening of the condition. Addressing CVI not only eases discomfort but also improves overall vein health.
Causes and Risk Factors of Chronic Venous Insufficiency
Understanding the causes of chronic venous insufficiency is vital. CVI often results from weak or damaged valves in the veins. This condition prevents normal blood flow back to the heart.
Several factors increase the risk of developing CVI. Knowing these can empower you to take preventive action.
Risk factors include:
- Age: People over 50 are more susceptible.
- Family history: Genetics can play a significant role.
- Obesity: Excess weight adds pressure to leg veins.
Additional risks are associated with prolonged periods of standing or sitting. Pregnancy and hormonal changes can also contribute to CVI development. Recognizing these factors aids in understanding your risk level.
By identifying these risks, you can make lifestyle changes to reduce your chances of developing CVI. Discussing concerns with a healthcare provider is always a wise step. Early awareness and intervention can improve long-term vein health.
Recognizing the Symptoms: Early and Advanced Stages
CVI presents various symptoms. Recognizing them early can lead to more effective treatment. Initially, symptoms might be mild and easily overlooked.
Early symptoms include:
- Leg swelling, especially in the ankles
- A feeling of heaviness in the legs
- Visible varicose veins
As the condition progresses, symptoms can worsen. You might experience increased leg pain or cramps. Skin changes, like dryness or discoloration, can also occur.
Advanced stages of CVI may lead to more serious complications. Skin ulcers may develop, often around the ankles. These ulcers can become infected if not treated promptly.
CVI symptoms can impact daily life. They may limit your ability to walk or stand for long periods. Identifying symptoms early and seeking medical advice are crucial steps. Doing so helps to manage the condition effectively and prevent progression.
Being aware of these symptoms empowers you to take control of your health. Seek professional guidance when changes in your symptoms occur.
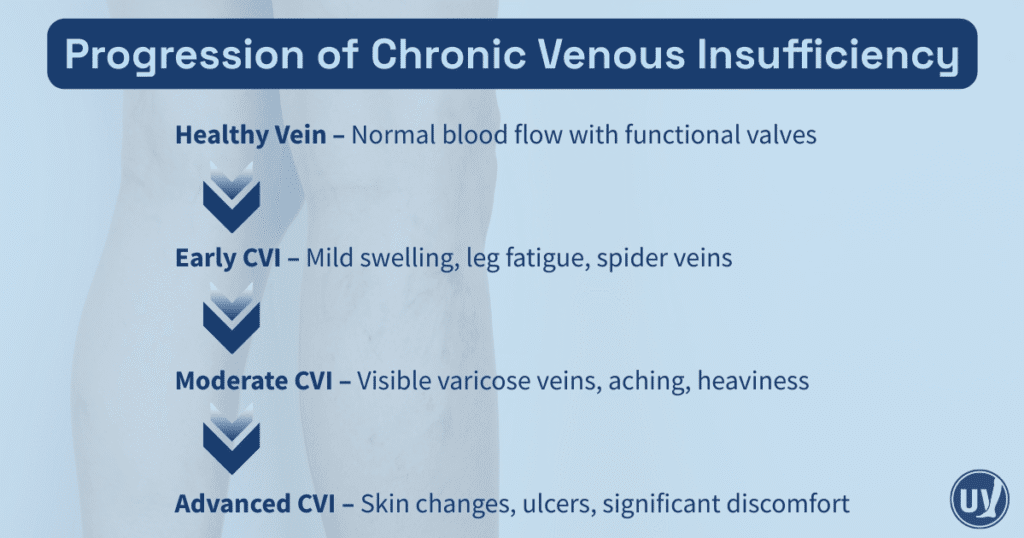
Understanding the Progression of Chronic Venous Insufficiency
CVI is a gradual condition. Understanding its progression helps in managing the disease effectively. Initially, symptoms might be slight and manageable.
In the early stages, symptoms such as leg heaviness might be misinterpreted as fatigue. As CVI advances, you may notice increased swelling and discomfort. This marks a progression from mild to moderate severity.
With time, untreated CVI can cause more serious issues. These might include persistent leg pain and skin changes. Additionally, the appearance of spider or varicose veins may become more prominent.
Leg Swelling Causes and How They Relate to CVI
Leg swelling is a common symptom of chronic venous insufficiency. This occurs when veins cannot effectively return blood to the heart. As a result, fluid accumulates, causing swelling.
Connecting leg swelling to CVI is vital. Swelling can signal worsening venous health. Early intervention and proper management are essential in preventing complications. Consulting a specialist ensures tailored care and effective treatment options.
Diagnosis: How Chronic Venous Insufficiency Is Identified
Diagnosing chronic venous insufficiency is a crucial step in managing the condition. A physical examination often serves as the starting point. Vein specialists assess symptoms like swelling and varicose veins.
Imaging tests, especially Doppler ultrasound, play a key role. This test evaluates blood flow and identifies problematic veins. Accurate imaging guides effective treatment planning.
Consulting a vein specialist ensures an accurate diagnosis and a personalized treatment strategy.
Venous Insufficiency Treatment Options
Treating chronic venous insufficiency involves multiple strategies. The goal is to alleviate symptoms and prevent complications. Treatment varies from lifestyle adjustments to medical interventions.
Lifestyle changes form the first line of defense. They are non-invasive and help manage mild symptoms. Regular physical activity and leg elevation can significantly aid circulation.
When lifestyle changes aren’t enough, compression therapy is recommended. Special stockings exert gentle pressure on the legs, helping blood return to the heart. This can reduce swelling and discomfort.
Minimally invasive procedures offer effective solutions for more severe cases. These treatments target the source of the issue, improving overall vein health. They are typically performed in an outpatient setting.
Consulting with a healthcare provider can determine the best treatment path. A personalized approach ensures the most effective results.
Preventing Progression and Complications
Taking proactive steps is crucial in managing chronic venous insufficiency. Early intervention can significantly slow its progression. By addressing CVI early, patients reduce their risk of serious complications.
Effective prevention strategies focus on lifestyle and medical management. Regular check-ups with a healthcare provider ensure timely adjustments to treatment plans. This approach aids in maintaining optimal vein health.
Important prevention strategies include:
- Adhering to prescribed treatment plans
- Regular monitoring by a healthcare professional
- Implementing consistent lifestyle changes
These measures help stabilize your condition and improve quality of life, ensuring complications are avoided.
When to See a Vein Specialist
Timely consultation with a vein specialist is essential when experiencing symptoms of chronic venous insufficiency. If you notice persistent leg swelling or discomfort, seek professional advice promptly.
Empowering Patients: Taking Charge of Your Vein Health
Knowledge is power when it comes to managing chronic venous insufficiency. By understanding your condition, you can make informed decisions and take proactive steps to protect your vein health. Staying informed, following a personalized treatment and lifestyle plan, and regularly consulting with a vein specialist can make a significant difference in your comfort and long-term results.
Your vein health doesn’t have to wait. Schedule a consultation with United Vein & Vascular Centers today to receive a comprehensive evaluation and learn which treatment options are right for you. Take the first step toward healthier, more comfortable legs.
Frequently Asked Questions
Early signs can include leg swelling, heaviness, fatigue, or visible spider veins. Noticing symptoms early allows for timely evaluation and intervention.
Lifestyle changes such as exercise, leg elevation, compression therapy, and careful monitoring can help manage CVI. Non-surgical procedures may also be recommended depending on your condition.
If you experience persistent swelling, aching, or skin changes in your legs, it’s important to schedule a consultation. Early evaluation can prevent complications and guide personalized treatment options.


