Contents
- Common Vein Conditions That Affect Circulation
- Early Signs of Vein Conditions Often Overlooked
- Unusual Areas Where Vein Conditions Can Develop
- Why Early Detection of Vein Conditions Matters
- Treatment Options and How Vein Conditions Are Managed
- Stay Ahead of Vein Issues With Early Care
- Frequently Asked Questions
Vein conditions can develop quietly and often begin long before symptoms become obvious. Many people focus on visible leg veins or occasional leg discomfort, but venous issues can appear in subtle ways throughout the body.
When veins cannot efficiently return blood to the heart, pressure increases and symptoms gradually surface. Recognizing these early indicators is an important step toward protecting long term vascular health and preventing complications.
Although vein conditions are frequently associated with the legs, the reality is much broader. Venous disorders range from cosmetic concerns to serious health issues that may require prompt attention. Understanding how these conditions develop and where symptoms may appear allows individuals to take early action and seek proper care.
Common Vein Conditions That Affect Circulation
A number of vein conditions impact how blood moves through the body. Each one develops differently, but all involve changes in venous pressure, damaged valves, or impaired circulation.
Varicose veins are one of the most recognized vein issues. These enlarged, twisted veins often appear on the legs and may cause heaviness, swelling, or throbbing sensations. Varicose veins develop when weakened valves allow blood to pool inside the vein, increasing internal pressure.
Spider veins are smaller and typically not painful, yet they are still a sign of venous dysfunction. These thin red, blue, or purple lines can appear on the legs, face, or other areas close to the surface of the skin.
Deep vein thrombosis, or DVT, occurs when a clot forms in a deep vein. This condition is a medical concern because a clot can break free and travel to the lungs, creating a life threatening pulmonary embolism. While DVT may sometimes present with swelling or pain, in many cases it shows few symptoms.
Chronic venous insufficiency is a condition in which the valves in the leg veins do not work properly. Blood has difficulty moving back toward the heart, causing swelling, aching, and skin changes around the lower legs.
Venous ulcers represent a more advanced stage of venous disease. These open wounds form when prolonged pressure and inadequate circulation prevent healing. They often develop near the ankles and require ongoing medical care.
Understanding these conditions provides context for the early signs that follow. Many symptoms start subtly, and identifying them early can make treatment more effective.
Early Signs of Vein Conditions Often Overlooked
Most early symptoms of vein disease begin in the legs, but they are not always obvious at first. Mild swelling around the ankles or lower legs often appears before visible veins develop. This swelling may worsen at the end of the day or after extended periods of sitting or standing.
A feeling of heaviness, fatigue, or discomfort in the legs can signal early circulation problems. Individuals may notice that their legs feel tired more quickly or that aches intensify even without strenuous activity.
Visible changes in the veins can also appear early. Small spider veins or thin, visible vessels may develop gradually and increase over time. While these veins may seem minor, they can indicate underlying pressure in the venous system.
Skin changes on the legs are also important to monitor. The skin may become dry, itchy, or slightly discolored. Over time, these changes may signal reduced circulation and the beginning stages of venous insufficiency.
Unusual Areas Where Vein Conditions Can Develop
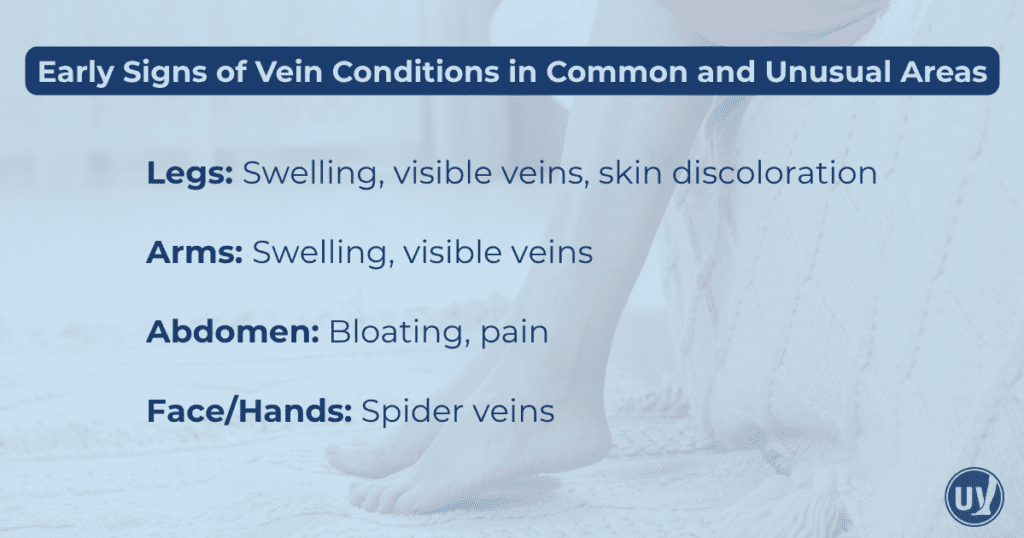
While the legs are the most common location for venous symptoms, vein issues can appear in less expected parts of the body. These signs are easier to overlook, yet can be equally important for early detection.
Some individuals notice swelling in one or both arms. Arm swelling can indicate a blockage, clot, or impaired circulation in the upper extremities, and it should not be ignored.
Visible veins on the arms, chest, or hands can also signal circulation changes. Although visible veins can be normal for some people, sudden changes in size, color, or pattern can indicate an underlying venous issue.
Certain abdominal symptoms may also relate to venous concerns. Unexplained abdominal pain, pressure, or bloating can sometimes result from changes in abdominal vein function. While these symptoms may have many causes, they should be evaluated when persistent.
Vein conditions can appear even around the face or eyes. Small spider veins on the face can be cosmetic, but in some cases they reflect increased venous pressure.
Being aware of symptoms in these unusual areas helps individuals recognize vein problems early, even when they do not match the typical image of varicose veins in the legs.
Why Early Detection of Vein Conditions Matters
Identifying vein conditions early significantly improves long term outcomes. When symptoms are recognized at an early stage, treatment can begin before the condition progresses into something more serious. Early care helps prevent complications such as skin breakdown, blood clots, or chronic pain.
Early detection also allows individuals to maintain a higher quality of life. Many people live with subtle venous symptoms without realizing how much they affect daily comfort. Addressing these issues early can help restore energy, reduce discomfort, and support an active lifestyle.
Treatment options are often simpler when started early. Minimally invasive procedures are highly effective for early stage vein conditions, offering short recovery times and strong long term results. As vein disease progresses, treatment may become more complex, which is why early evaluation is so valuable.
Treatment Options and How Vein Conditions Are Managed
Treatment for vein conditions depends on the severity of the symptoms and the specific diagnosis. In many cases, lifestyle changes play an important role. Regular physical activity supports healthy circulation and strengthens the muscles that help move blood through the veins. Maintaining a balanced diet and a healthy weight can also reduce pressure on the venous system.
Compression stockings are often recommended to reduce swelling and discomfort. These garments help blood move more efficiently and alleviate many early symptoms.
Medical treatment options are available for both cosmetic and more advanced vein issues. Sclerotherapy is a popular option for spider veins and small varicose veins. It involves injecting a solution that causes the vein to close and fade.
Laser therapy uses light energy to treat small veins near the surface of the skin. This method is minimally invasive and requires no incisions.
For larger or more advanced vein conditions, endovenous ablation may be recommended. This treatment uses heat to close unhealthy veins and redirect blood to healthier pathways. Other conditions may benefit from medical procedures such as angioplasty and stenting, which open narrowed or blocked veins.
A vein specialist can evaluate symptoms, identify the underlying cause, and recommend the right treatment approach.
Stay Ahead of Vein Issues With Early Care
Vein conditions can affect daily comfort and long term health, but early awareness makes a significant difference. Paying attention to early signs in both common and unusual areas helps prevent progression and ensures that treatment remains simple and effective. Whether you have noticed changes in your legs, arms, abdomen, or other areas, taking action now can protect your health for years to come.
If you are experiencing symptoms or have concerns about your vein health, the specialists at United Vein and Vascular Centers are ready to help. Schedule a consultation to receive expert evaluation and personalized treatment options that support your long term well being.
Frequently Asked Questions
Early signs include swelling, discoloration, visible small veins, or a feeling of heaviness and fatigue in the area.
Early detection helps prevent complications such as chronic venous insufficiency, blood clots, or worsening varicose veins. Treating vein conditions early often allows for less invasive interventions.
If you notice unexplained swelling, discoloration, pain, or bulging veins, especially in unusual areas, it’s best to schedule an evaluation. A vein specialist can diagnose the issue and guide you toward the right treatment plan.


