Blood circulation is essential for sustaining life. It delivers oxygen and nutrients to tissues and organs while removing waste products. This complex system is made up of arteries, veins, and capillaries. Arteries carry oxygen-rich blood away from the heart to nourish the body, while veins return oxygen-depleted blood back to the heart. Capillaries, the smallest blood vessels, facilitate the exchange of oxygen, nutrients, and waste between blood and tissues. Any disruption in this process can lead to vascular diseases, which can be categorized into arterial and venous conditions. Understanding how these systems work is key to maintaining overall circulatory health and preventing serious complications.
How Circulation Affects Your Health
When blood circulation is working properly, every tissue in the body receives adequate oxygen and nutrients, which are essential for energy production and healthy cellular function. If circulation is compromised, organs and tissues may not get the oxygen they need. This can lead to dysfunction and disease. Circulatory problems range in severity, from mild issues such as temporary numbness or tingling to more serious complications like chronic pain, non-healing wounds, or ulcers. Maintaining healthy circulation through lifestyle choices and medical care is critical to reducing the risk of developing these conditions.
Arterial Disease Explained
Arterial disease, often referred to as peripheral artery disease or PAD, occurs when arteries become narrowed or blocked. This reduces blood flow from the heart to the limbs and other parts of the body. The narrowing usually results from the buildup of plaque, which is made up of cholesterol, fatty substances, calcium, and other cellular debris. Plaque hardens over time, causing arteries to lose elasticity and making them more prone to blockages. Reduced blood flow can also lead to the formation of blood clots, which further impede circulation.
Arterial disease can affect any artery in the body, including those supplying the heart and brain, leading to conditions such as coronary artery disease or increasing the risk of stroke. In the legs and feet, PAD often causes pain and mobility difficulties. If left untreated, PAD can progress to a severe condition called critical limb ischemia, which may require amputation. Early detection and management are crucial to prevent serious outcomes and preserve quality of life.
Causes and Risk Factors for Arterial Disease
The primary cause of arterial disease is atherosclerosis, the accumulation of plaque in the arterial walls. Several risk factors contribute to this process. Smoking damages blood vessels and accelerates plaque formation. High cholesterol and high blood pressure increase the likelihood of plaque buildup. Diabetes, obesity, and a sedentary lifestyle also contribute to arterial disease.
Genetics play an important role, and a family history of heart disease can increase susceptibility. Age is another factor, as the risk of arterial disease rises over time. Environmental and lifestyle factors, including chronic stress and unhealthy eating habits, can further elevate the risk. Addressing these factors through lifestyle changes and medical management can significantly reduce the chances of developing arterial disease.
Symptoms of Arterial Disease
Common signs of arterial disease include leg pain or cramping during physical activity, numbness or weakness in the legs, coldness in the lower legs or feet, and sores or wounds on the toes, feet, or legs that do not heal. These symptoms occur because oxygen-rich blood cannot reach the muscles and tissues effectively. Intermittent claudication, which is pain that occurs during exercise and subsides with rest, is a common early sign. As the disease progresses, symptoms may persist, signaling a worsening condition.
Advanced arterial disease can lead to critical limb ischemia, which is characterized by severe pain even at rest, non-healing wounds, and tissue death. This highlights the importance of early recognition and timely intervention to prevent irreversible damage.
Treatment Options for Arterial Disease
Treatment for arterial disease focuses on restoring and improving blood flow. Lifestyle modifications play a key role. Quitting smoking, exercising regularly, and controlling cholesterol and blood pressure are essential steps. These changes help manage symptoms and slow the progression of plaque buildup in the arteries.
Medications may also be prescribed. Cholesterol-lowering drugs, blood thinners, and medications to manage blood pressure and diabetes are commonly used. These help prevent blood clots, reduce plaque formation, and improve overall cardiovascular health. In severe cases, procedures such as angioplasty or bypass surgery may be necessary. Angioplasty widens narrowed arteries using a balloon, while bypass surgery creates a new route for blood flow around blocked vessels.
Understanding Venous Disease
While arterial disease involves the arteries, venous disease affects the veins, which are responsible for returning blood to the heart. One of the most common venous conditions is chronic venous insufficiency, or CVI. In CVI, the valves within the veins fail to function properly, allowing blood to pool and increasing pressure within the veins.
This pooling can cause swelling and discomfort and often leads to varicose veins, which are enlarged and twisted veins visible just under the skin. Venous disease can also result in more serious complications, including deep vein thrombosis and venous ulcers. Understanding venous disease is critical for preventing these complications and maintaining healthy veins.
Causes and Risk Factors for Venous Disease
Venous disease can result from damage to the vein walls or valves. Family history, obesity, pregnancy, prolonged sitting or standing, and age are all risk factors. These elements weaken the vein walls and valves, making it harder for blood to return to the heart efficiently.
Hormonal changes, particularly in women, can also increase the risk of venous disease. Occupations that require long periods of standing or sitting can exacerbate symptoms by reducing natural blood flow. Lifestyle factors such as lack of exercise and poor diet further contribute to the risk. Recognizing these factors allows individuals to take proactive steps to maintain vein health.
Symptoms of Venous Disease
The signs of venous disease include swelling in the legs or ankles, a feeling of heaviness or aching in the legs, visible varicose veins, and changes to the skin or development of ulcers. These symptoms result from increased venous pressure and inadequate return of blood to the heart. Swelling, or edema, is often the first noticeable symptom. As the disease progresses, the skin may discolor or develop sores due to poor circulation.
In more severe cases, venous disease can lead to thrombophlebitis, where veins become inflamed because of blood clots. Early recognition of symptoms enables timely intervention, preventing progression and reducing the risk of complications.
Treatment for Venous Disease
Treatment for venous disease focuses on relieving symptoms and preventing complications. Compression therapy, often with specially designed stockings, helps improve circulation by applying pressure to the legs. Lifestyle adjustments such as maintaining a healthy weight, elevating the legs, and exercising regularly support better blood flow and reduce pressure on the veins.
In some cases, medical procedures may be necessary. Sclerotherapy involves injecting a solution into a vein to collapse it, while laser treatments use focused light to close off problematic veins. Surgical options are reserved for more severe cases when other treatments are not effective. Combining medical interventions with lifestyle changes can significantly improve quality of life for individuals with venous disease.
Key Differences Between Arterial and Venous Disease
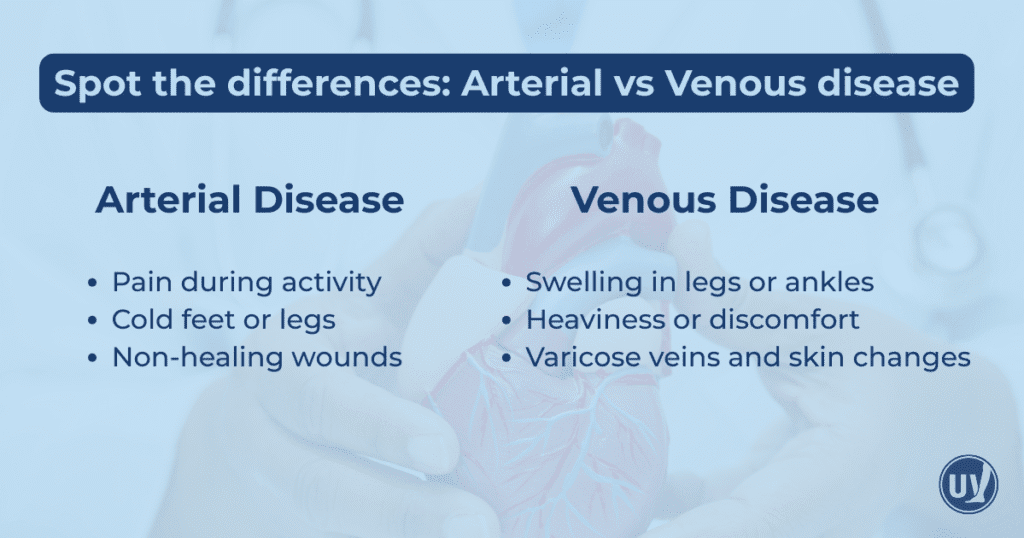
Although both arterial and venous diseases affect circulation, they differ in causes, symptoms, and treatments. Arterial disease results from narrowed arteries due to plaque buildup, reducing blood flow to the limbs. Venous disease stems from valve dysfunction, causing blood to pool in the veins.
Arterial disease often presents with pain during exercise, cold limbs, and wounds that do not heal. Venous disease typically causes swelling, heaviness, varicose veins, and skin changes. Recognizing these differences is essential for accurate diagnosis and effective treatment.
Managing and Preventing Circulatory Diseases
Both arterial and venous conditions benefit from lifestyle modifications and medical care, but the approaches differ. Arterial disease treatments focus on improving blood flow through medications and procedures that address plaque buildup. Venous disease management emphasizes supporting vein function, relieving pressure, and preventing complications.
Early intervention is critical. Anyone experiencing symptoms related to arterial or venous disease should seek evaluation from a healthcare provider who specializes in vein and vascular conditions. Timely medical attention can prevent disease progression, alleviate symptoms, and improve overall health and quality of life.
Taking Control of Your Vascular Health
Understanding the differences between arterial and venous disease empowers patients to make informed healthcare decisions. Maintaining a healthy lifestyle, adhering to prescribed treatment plans, and consulting with vein specialists at United Vein & Vascular Centers can protect your circulation and prevent serious complications. Proactive management of vascular health ensures better long-term outcomes, allowing you to maintain mobility, comfort, and overall well-being.
Taking charge of your vascular health is an investment in your quality of life. If you notice signs of arterial or venous disease, contact a UVVC clinic to schedule a personalized evaluation and care plan. Early attention can make a profound difference in your health and provide peace of mind as you safeguard your circulation for years to come.
Frequently Asked Questions
Arterial disease occurs when arteries narrow due to plaque buildup, reducing blood flow to the limbs. Venous disease happens when vein valves fail, causing blood to pool and leading to swelling, varicose veins, or ulcers.
Arterial disease often causes leg pain during activity, cold feet, or non-healing wounds. Venous disease may cause leg swelling, heaviness, varicose veins, or skin changes such as discoloration or ulcers.
Maintaining a healthy lifestyle with regular exercise, balanced diet, and weight management, avoiding smoking, and seeking early evaluation from a vein specialist can reduce your risk of both arterial and venous conditions.


