Contents
- What Is Peripheral Artery Disease
- Symptoms and Risk Factors of PAD
- Diagnosing PAD
- Treatment Options for PAD
- What Is Angioplasty
- Stents in Legs
- Angioplasty Compared to Catheterization
- The Angioplasty and Stenting Procedure
- Benefits and Risks
- Recovery and Aftercare
- Take the Next Step with UVVC
- Frequently Asked Questions
Peripheral artery disease, or PAD, affects millions of people and occurs when arteries become narrowed or blocked, reducing blood flow to the limbs. This reduction can cause pain, cramping, and difficulties with mobility. Angioplasty and stenting are among the most common treatments for PAD, helping restore circulation and improve quality of life. Understanding these procedures, how they work, and what to expect during recovery is essential for anyone affected by PAD. This article provides a comprehensive look at angioplasty, stenting, and emerging treatment options.
What Is Peripheral Artery Disease
Peripheral artery disease is a circulatory condition in which fatty deposits, called plaque, build up in the arteries. This narrowing limits the amount of blood flowing to the limbs, most often the legs. Reduced blood flow can lead to pain during walking or exercise, muscle fatigue, and in severe cases, tissue damage.
PAD often goes undiagnosed because its early symptoms may resemble other conditions. Recognizing the warning signs is critical for timely treatment. Without intervention, PAD can result in serious complications, including non-healing wounds or even limb loss.
The primary cause of PAD is atherosclerosis, the accumulation of fatty deposits inside the arteries. Risk factors that contribute to PAD include smoking, diabetes, high blood pressure, and elevated cholesterol. Being aware of these factors can help with early detection and prevention. Individuals who suspect they may have PAD should consult a healthcare professional to determine the most appropriate treatment plan.
Symptoms and Risk Factors of PAD
PAD symptoms vary depending on severity. One of the most common signs is leg pain or cramping during physical activity, a condition known as claudication. This pain typically eases with rest but returns with exertion. Other symptoms can include numbness, weakness, or coldness in the legs, and sores on the toes or feet that heal slowly.
Lifestyle choices, such as smoking and poor diet, can increase the risk of developing PAD. Chronic health conditions, including diabetes, high blood pressure, and high cholesterol, are also significant contributors. Recognizing these risks can help patients take steps to reduce the likelihood of disease progression. Quitting smoking, maintaining a balanced diet, staying physically active, and attending regular medical check-ups can all support vascular health.
Diagnosing PAD
Diagnosing PAD involves a combination of reviewing patient history, conducting a physical examination, and performing diagnostic tests. Physicians assess symptom patterns, evaluate risk factors, and may use imaging studies to visualize blood flow.
A common diagnostic tool is the ankle-brachial index, or ABI. This test compares blood pressure in the ankle to that in the arm to determine if blood flow is restricted. Abnormal results can indicate blockages and confirm the presence of PAD. Additional tests may include ultrasound imaging, magnetic resonance angiography, or computerized tomography angiography. These evaluations help physicians determine the severity of PAD and develop a personalized treatment plan.
Treatment Options for PAD
The goal of PAD treatment is to restore blood flow, relieve symptoms, and prevent complications. The approach depends on the severity of the disease and the overall health of the patient.
Non-invasive treatments often start with lifestyle modifications and medications. Exercise programs, dietary changes, and quitting smoking are all recommended. Medications may include cholesterol-lowering drugs, blood thinners, or medications to improve circulation.
When lifestyle changes and medication are not sufficient, direct interventions may be necessary. Angioplasty and stenting are minimally invasive procedures that open blocked arteries. Bypass surgery redirects blood flow around obstructed vessels, while atherectomy removes plaque from artery walls. Working with a healthcare provider to select the most suitable treatment is crucial for achieving optimal outcomes.
What Is Angioplasty
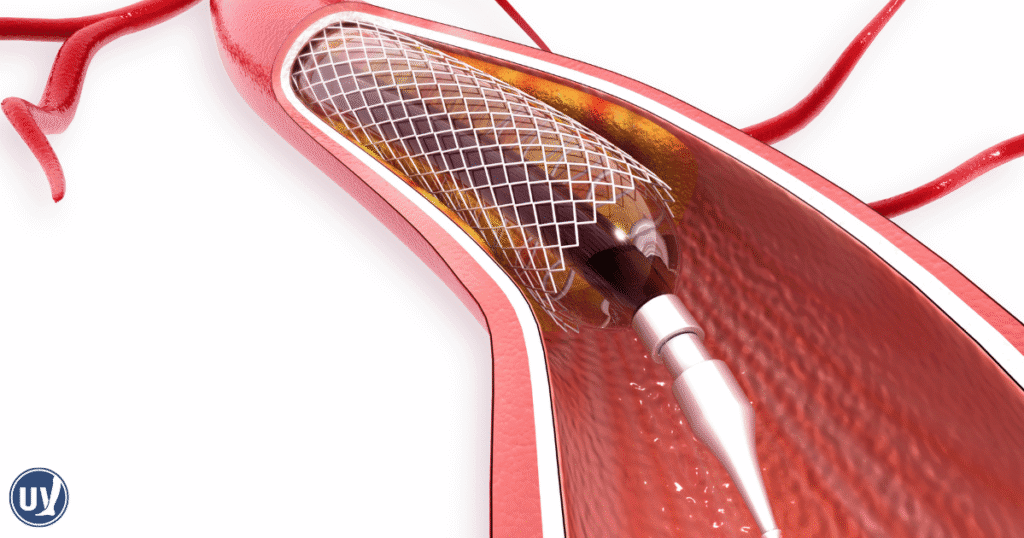
Angioplasty is a procedure designed to widen narrowed or blocked blood vessels. It is commonly used to treat blockages in the arteries of the legs caused by PAD. During the procedure, a thin catheter with a balloon at its tip is inserted into the affected blood vessel. The balloon is then inflated to expand the artery and restore blood flow.
Angioplasty can be combined with stenting, where a small metal mesh tube is inserted to keep the artery open. This approach reduces the chance of the artery narrowing again. Angioplasty is typically performed on an outpatient basis, offering a minimally invasive option with quicker recovery than traditional surgery.
Stents in Legs
Stents are small wire mesh tubes that provide support to arteries after angioplasty. When placed inside a narrowed artery, the stent acts as a scaffold, holding the vessel open and improving circulation. Stents are permanent and designed to adapt to natural body movements, enhancing mobility and reducing symptoms.
The use of stents provides long-term support for artery walls and helps prevent re-narrowing. Patients often experience relief from pain and improved leg function following stent placement.
Angioplasty Compared to Catheterization
Angioplasty and catheterization are different procedures that are sometimes confused. Catheterization is mainly diagnostic, used to examine arteries and identify blockages. Angioplasty is therapeutic, focusing on widening the arteries to improve blood flow.
Catheterization is exploratory, while angioplasty actively treats arterial narrowing. Understanding these distinctions allows patients to make informed choices about their care and manage PAD effectively.
The Angioplasty and Stenting Procedure
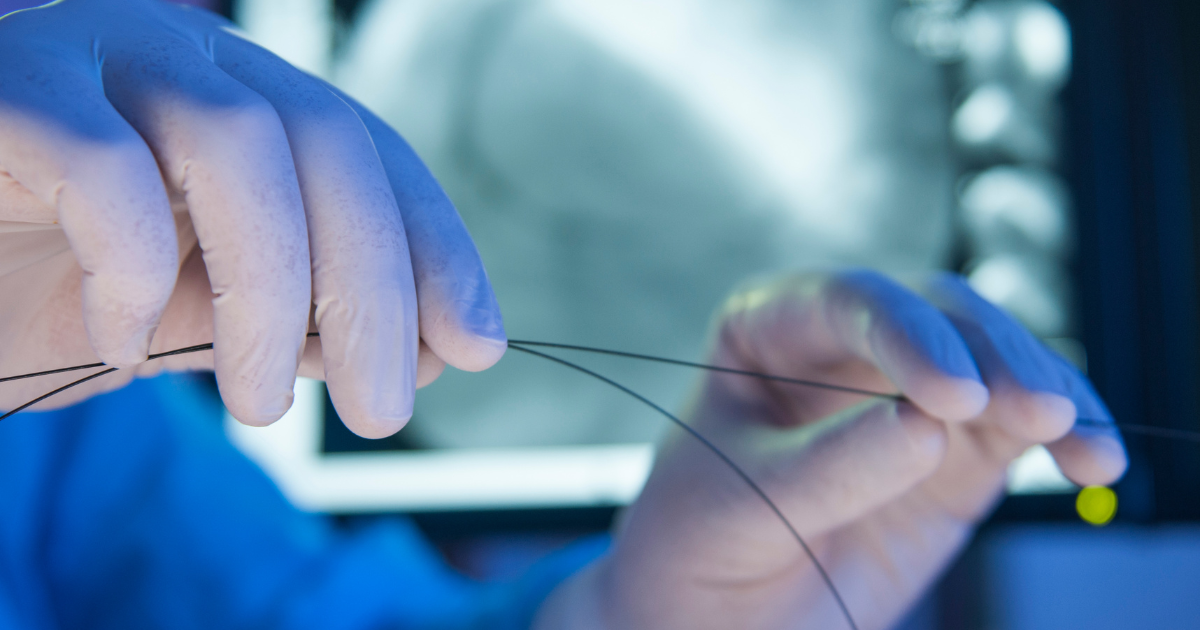
The procedure begins with a small incision in the groin or arm to access the blood vessel. A contrast dye is injected to visualize the artery on X-ray images. A balloon-tipped catheter is then guided to the narrowed section, and the balloon is inflated to expand the artery.
If needed, a stent is placed to keep the artery open. The balloon is deflated and removed, leaving the stent in place. The entire process typically takes less than two hours and is minimally invasive, allowing for a quicker recovery compared to traditional surgeries.
Benefits and Risks
Angioplasty and stenting offer significant benefits for patients with PAD. They can relieve leg pain, improve mobility, and enhance overall quality of life. Recovery is generally faster than with open surgery, and most patients see substantial symptom relief.
However, risks exist. Potential complications include bleeding, infection, or damage to the artery. Despite these risks, angioplasty and stenting have high success rates and are widely used to treat PAD. Follow-up care is essential to monitor outcomes and ensure long-term health.
Recovery and Aftercare
Recovery from angioplasty and stenting is typically straightforward. Most patients return home the same day and gradually resume daily activities. Patients should avoid strenuous activity initially and monitor the insertion site for signs of infection.
Follow-up appointments allow healthcare providers to evaluate treatment success. Lifestyle changes, such as exercise and dietary adjustments, complement medical care and help maintain long-term vascular health. Adhering to medical advice ensures effective management of PAD.
Take the Next Step with UVVC
Managing PAD effectively requires a combination of medical care, lifestyle adjustments, and patient education. Angioplasty and stenting are safe and effective options for many patients. If you or a loved one is experiencing symptoms of peripheral artery disease, schedule a consultation with United Vein and Vascular Centers today. Our experienced team can evaluate your condition, discuss treatment options, and help you take control of your vascular health.
Frequently Asked Questions
Most patients report minimal discomfort during angioplasty. Sedation and local anesthesia are used to keep the procedure comfortable.
Recovery is usually quick. Many patients return home the same day and gradually resume normal activities over a few days.
Stents are designed to be permanent. Modern stents are durable and adapt to natural movements, helping maintain improved blood flow long-term.