Contents
- Why Vein Symptoms Are Often Overlooked
- Vein Symptoms You Should Never Ignore
- Why Vein Disease Worsens Without Treatment
- When It’s Time to See a Specialist
- How Vein Specialists Evaluate Symptoms
- Treatment Options for Symptomatic Vein Disease
- Frequently Asked Questions
- When To Seek Care and How UVVC Can Help
Many vein-related symptoms start subtly. A little swelling at the end of the day. Legs that feel heavier than they used to. A vein that’s more noticeable than last year. Because these changes often develop gradually, they’re easy to dismiss as part of aging, stress, or long days on your feet.
But vein disease is progressive, and certain symptoms should never be ignored. Recognizing warning signs early can help prevent complications, reduce discomfort, and lead to more effective treatment options.
This guide breaks down the vein symptoms that deserve medical attention and explains when it’s time to see a specialist.
Why Vein Symptoms Are Often Overlooked
Vein disease affects millions of people, yet many delay care because:
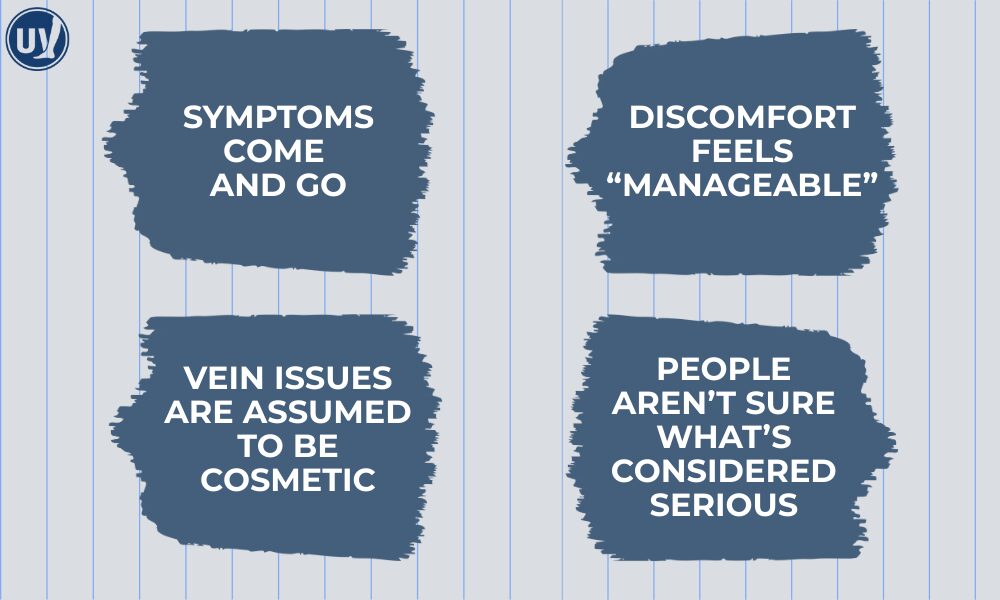
Unfortunately, waiting can allow underlying circulation problems to worsen.
Conditions like chronic venous insufficiency (CVI) and varicose veins don’t usually resolve on their own. Instead, they tend to progress gradually, making early evaluation especially important.
Vein Symptoms You Should Never Ignore
While not every symptom indicates an emergency, certain signs consistently point to vein disease that should be evaluated by a specialist.
Persistent leg swelling
Occasional swelling after long travel or a busy day can be normal. But ongoing or recurring leg swelling, especially if it worsens throughout the day, may signal poor venous circulation.
When veins struggle to return blood to the heart, fluid can leak into surrounding tissues, causing swelling in the lower legs or ankles.
Swelling is often associated with:
- Chronic venous insufficiency
- Varicose veins
- Prolonged standing or sitting
- Worsening circulation over time
If swelling becomes routine or affects one leg more than the other, it should be evaluated.
Leg Heaviness, Aching, or Fatigue
Legs that feel heavy, tired, or achy, particularly at the end of the day, are one of the most common CVI symptoms.
This discomfort often:
- Worsens with prolonged standing or sitting
- Improves with leg elevation
- Returns daily or weekly
- Progresses over time
Heaviness is not just discomfort; it reflects increased pressure inside the veins.
Bulging or Increasingly Visible Veins
Visible varicose veins are more than a cosmetic concern. They indicate underlying vein valve dysfunction that allows blood to pool.
You should not ignore veins that:
- Appear larger or more twisted over time
- Become tender or warm
- Are accompanied by pain or swelling
- Limit your activity or comfort
Nighttime Leg Cramps or Restlessness
Frequent leg cramps, aching, or restlessness at night can be linked to vein disease.
Poor circulation can lead to:
- Muscle fatigue
- Reduced oxygen delivery
- Cramping during rest
- Difficulty sleeping
If cramps occur regularly, especially alongside swelling or heaviness, vein disease may be contributing.
Skin Changes on the Lower Legs

Changes in skin texture or color around the ankles or lower legs should never be ignored. These changes often signal long-standing venous pressure.
Watch for:
- Darkening or discoloration
- Dry, itchy, or irritated skin
- Thickening or hardening of tissue
- Redness or inflammation
These signs suggest advancing venous disease and increase the risk of ulcers if untreated.
Leg Pain That Worsens Over Time
Vein-related pain may start mild but gradually intensify. Pain that:
- Persists despite rest
- Interferes with daily activities
- Limits walking or standing
- Feels worse at the end of the day
deserves evaluation. Progressive pain is a key indicator that vein disease may be worsening.
Sudden Swelling, Warmth, or Pain in One Leg
This is one symptom that requires urgent medical attention.
Sudden leg swelling, warmth, redness, or pain, especially in one leg, may indicate deep vein thrombosis (DVT), a serious condition involving a blood clot.
If these symptoms appear suddenly, seek care immediately.
Why Vein Disease Worsens Without Treatment
Vein disease is progressive because damaged vein valves do not repair themselves. Over time:
- Vein walls stretch
- Valve function declines
- Blood pooling increases
- Pressure damages surrounding tissue
Early evaluation allows specialists to intervene before complications develop.
When It’s Time to See a Specialist
You should consider scheduling a vein evaluation if:
- Symptoms persist for weeks or months
- Discomfort affects daily activities or sleep
- Swelling or pain worsens over time
- Visible veins continue to progress
- Skin changes appear near the ankles
- Home remedies no longer help
Seeing a specialist doesn’t mean committing to treatment — it provides clarity and guidance.
How Vein Specialists Evaluate Symptoms
A comprehensive vein evaluation typically includes a review of your medical history, a physical examination, and a detailed discussion of your symptoms and how they’ve changed over time. Diagnostic ultrasound imaging is also used to assess blood flow and identify underlying circulation issues. Together, these steps allow specialists to determine whether your symptoms are vein-related and which treatment options may be most appropriate.
Treatment Options for Symptomatic Vein Disease
Modern vein treatments are minimally invasive and performed in-office.
Common options include:
- VenaSeal™ – Medical adhesive to close diseased veins
- Radiofrequency Ablation (RFA) – Uses controlled heat to seal faulty veins
- Microphlebectomy – Removes bulging surface veins through small incisions
- Sclerotherapy – Treats spider veins and small varicose veins
- Varithena® – Uses microfoam to treat varicose veins caused by venous reflux
Treatment selection depends on vein size, location, symptoms, and circulation findings.
Frequently Asked Questions
Swelling that is persistent, worsening, or occurs suddenly, especially in one leg, should be evaluated, as it may signal vein disease or a clot.
Yes. Ongoing heaviness or aching is a common symptom of chronic venous insufficiency and should not be ignored.
Bulging veins often indicate vein valve dysfunction and underlying circulation problems.
They can be. Poor circulation may contribute to nighttime cramping or restlessness.
Yes. Skin changes around the ankles are often linked to long-standing venous pressure and should be evaluated.
When To Seek Care and How UVVC Can Help
If you’re experiencing leg swelling, heaviness, visible veins, or skin changes, it may be time for a professional evaluation. Early care can help prevent progression and improve daily comfort.
At United Vein & Vascular Centers, our specialists provide comprehensive evaluations and personalized treatment plans using advanced, minimally invasive techniques.
Find a clinic near you and schedule your consultation today.


