Contenido
- “Why do wounds on the lower leg or ankle heal so slowly, and what does that tell us medically?”
- Q: Why do wounds on the lower leg or ankle heal more slowly than other areas?
- Q: What’s the difference between a venous ulcer and a diabetic ulcer?
- Q: How does chronic venous insufficiency contribute to skin discoloration or tissue damage?
- Q: When should someone see a wound care specialist instead of treating at home?
- What’s Next in the Ask the Doc Series
Welcome to Ask the Doc, a new educational series from United Vein & Vascular Centers designed to bring clarity, confidence, and medically grounded answers to the vein-health questions patients ask most. Each week, a UVVC physician will break down essential topics surrounding vein and vascular care, what symptoms matter, when to seek help, and how modern minimally invasive treatments can restore comfort and mobility with minimal downtime.
In this installment, Dr. Loan Lam answers a frequently misunderstood question:
“Why do wounds on the lower leg or ankle heal so slowly, and what does that tell us medically?”
Dr. Lam’s insights reinforce UVVC’s commitment to medical leadership, advanced diagnostic imaging, and comprehensive vascular care.
Q: Why do wounds on the lower leg or ankle heal more slowly than other areas?
Dr. Lam:
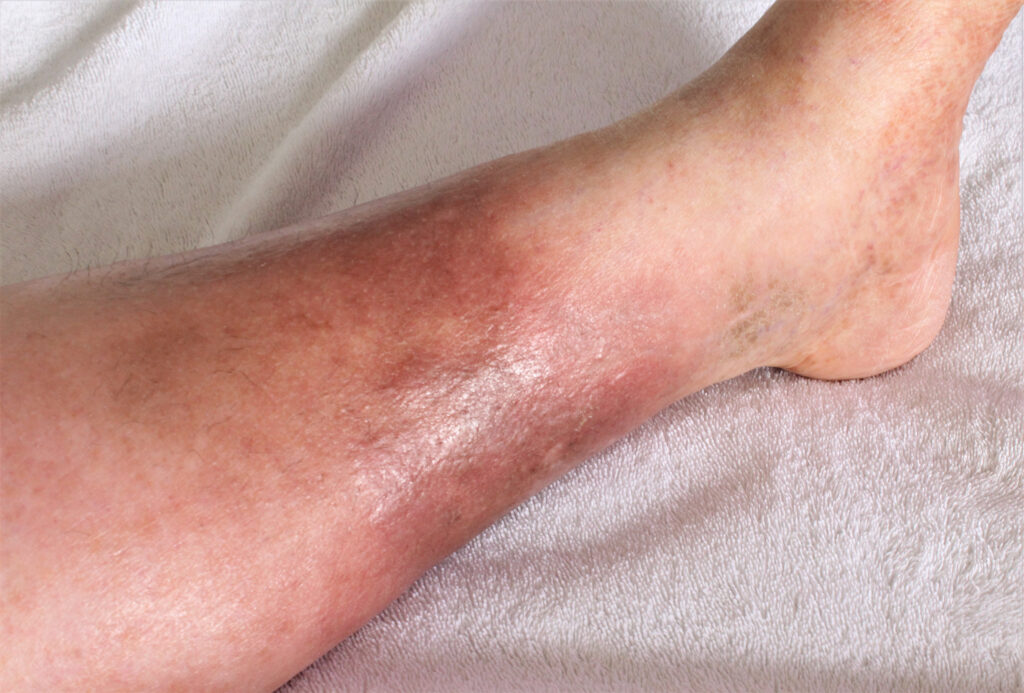
Wounds on the lower leg heal more slowly because this region has a higher demand for healthy circulation. Your body needs oxygen, nutrients, and immune support to repair damaged tissue. When blood flow is compromised, even a minor injury can become a lingering problem.
One of the most common reasons for slow healing is chronic venous insufficiency (CVI). When the valves in the veins weaken, blood falls backward and pools in the lower legs. This increased pressure inflames the tissue, makes the skin fragile, and reduces the body’s ability to heal injuries efficiently.
Other factors, such as diabetes, swelling, reduced mobility, and age, can also contribute, but venous disease is often the primary driver.
Q: What’s the difference between a venous ulcer and a diabetic ulcer?
Dr. Lam:
Both are slow-healing wounds, but they arise from very different issues:
Venous Ulcers
- Caused by venous insufficiency
- Commonly appear near the inner ankle
- Surrounding skin may look darkened, shiny, or hardened
- Often accompanied by swelling or visible varicose veins
These wounds occur because constant venous pressure weakens the skin until it breaks down.
Diabetic Ulcers
- Linked to poor arterial circulation and loss of sensation (neuropathy)
- Frequently found on the feet, toes, or pressure points
- Patients may not feel pain, so the wound can progress unnoticed
- Higher risk of infection
Some patients actually have mixed ulcers, meaning both venous and arterial factors contribute. That’s why a proper diagnosis is essential. Treating the wrong cause leads to poor outcomes.
Q: How does chronic venous insufficiency contribute to skin discoloration or tissue damage?
Dr. Lam:
CVI causes sustained pressure in the veins. Over time, red blood cells and iron pigments leak into the surrounding tissue, creating brownish or reddish discoloration around the ankles, known as hemosiderin staining. This isn’t just a cosmetic issue; it’s a sign of chronic inflammation and impaired skin health.
As venous disease progresses, the skin may become:
- thin or fragile
- itchy
- tight or hardened (lipodermatosclerosis)
- more susceptible to injury
When the skin loses its resilience, even minor trauma, like bumping your shin, can produce a wound that becomes difficult to heal without addressing the underlying circulation problem.
Q: When should someone see a wound care specialist instead of treating at home?
Dr. Lam:
You should seek a medical evaluation if:
- A wound isn’t improving after 1–2 weeks
- It becomes larger, deeper, or more painful
- You notice drainage, odor, or redness
- The surrounding skin is darkening or hardening
- Swelling persists or worsens
- You have diabetes, venous disease, or circulation problems
Slow-healing wounds are rarely just skin-deep. They often reflect underlying venous or arterial issues, and treating the wound alone, without treating the cause, leads to recurrence. A wound care specialist can determine why the wound developed and create a plan that promotes real healing.
What’s Next in the Ask the Doc Series
Ask the Doc offers clear, medically grounded explanations about the full spectrum of vein and vascular health. Every week, a UVVC physician breaks down key topics to help you understand your symptoms, your circulation, and your treatment options.
Next week, Dr. Shannon Davis will explain why nighttime leg aching is so common and when those symptoms should prompt a specialist evaluation. If you’re considering care now, visit our Find a Clinic page to schedule an appointment at a UVVC location near you.
Medically reviewed by UVVC National Medical Director, Dr. Domenic Zambuto




